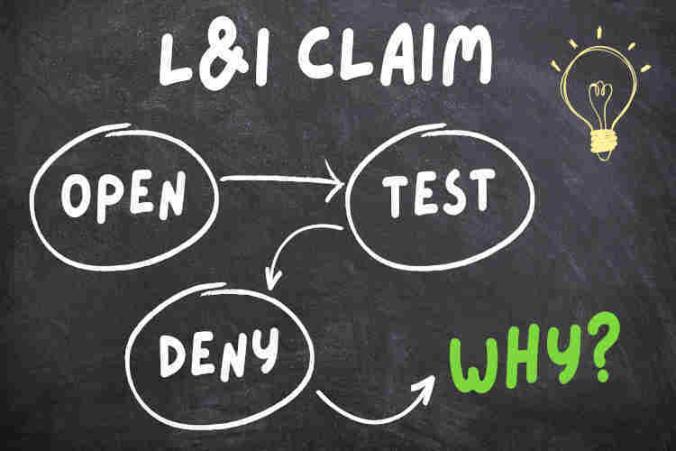
Every L&I claim is different. The conditions and circumstances of each workers’ compensation claim are unique. However, many L&I claim cases follow a similar process.
A common process and pattern in L&I claims
Most L&I claims that come across my desk follow the same pattern. More explicitly, the pattern consists of the following steps:
1. A doctors diagnoses the injury as sprain or strain
2. The attending provider prescribes physical therapy
3. Doctors perform clinical exams
4. Medical providers proceed with diagnosis studies
5. L&I subscribes the worker to a pain management program
6. Doctors identify more complex diagnosis
7. L&I sends the worker to an independent medical exam (IME)
8. L&I closes the claim because of pre-existing conditions.
Too many claims follow this L&I claim process, blindly. Many workers fall in a gray area. They do not receive what they deserve under the law. The purpose of this article is to explain the L&I claim process and the steps above. Hopefully, workers can figure out where they stand in the process and decide what to do next.
Work injury happens
A worker suffers an injury on the job. Usually, the injury isn’t visible. However, there’s no question that the worker is in pain. Sometimes, the worker goes to the emergency room (ER) or urgent care right away. Other times, they wait several days. Most commonly, workers hope that the problem will go away on its own.
Sprain or strain diagnosis
The first step in the L&I claim process is when the worker first sees a doctor for the work injury. Usually, the doctor diagnoses the worker with a sprain or strain. A sprain or a strain is a soft tissue injury. It includes muscle injury and injury of the tendons. The treatment for sprain or strain diagnosis typically includes:
Sometimes, a doctor orders an x-ray of the affected body part. An x-ray can help determine the diagnosis. On top, it can rule out a fracture. If there’s no fracture, then doctors expect sprains and strains to resolve quickly. Typically, with minimal treatment.
Physical therapy
On occasion, the worker continues to complain about pain. In actuality, there’s no real medical improvement. Then, doctors typically prescribe physical therapy. Some attending providers also call for more diagnostics, such as an MRI. Yet, in my experience, L&I denies MRI exams early in the workers’ compensation claim process. Normally, L&I wants workers to at least attempt physical therapy.
However, many times pain complaints continue. Moreover, physical therapy doesn’t always improve the worker’s pain. That’s when things can start getting messy in your L&I claim process.
What happens in my L&I claim if physical therapy doesn’t help
Say that rest, activity modification, pain medication and physical therapy are not helpful. Next, doctors usually look for signs of more serious problems. Here, doctors may perform certain clinical exam and tests. It all depends on the body part and suspected condition. L&I considers these exam results to be objective medical evidence. For example, say the work injury claimant has persistent low back pain. Then, doctors may perform a straight leg raise exam. This exam checks for potential radiculopathy or nerve impingement.
Additionally, there are other tests that we call “provocative tests”. They help doctors determine more complex workplace injuries. Examples of such complex injuries include:
a) Elbow, wrist, or shoulder impingement
b) Knee and shoulder tear
c) Other spinal disc herniation or displacement
If provocative tests suggest a medical problem, then doctors order more diagnostic studies. Frequently, they include imaging studies. For example, MRI tests and CT scans. Also, doctors often order nerve conduction studies like EMG.
Pain management program (SIMP) and work conditioning
In an L&I claim, the Department of Labor and Industries (L&I) considers pain complaints as subjective. In contrast, diagnostic results are objective. However, objective diagnostics may not explain subjective symptoms and complaints. In such instances, L&I can refer the work injury claimant to an L&I pain management program like SIMP. Or, to a work conditioning or work hardening program. Typically, this is the final treatment attempt before claim closure.
A serious diagnosis & causation
Alternatively, a diagnostic study may objectively find more serious problems. If that’s the case, then causation is going to be the next issue in your L&I claim. There are several serious conditions that doctors often detect through MRI, CT scan or EMG. The list of serious problems we see in L&I claims at our office includes:
1) Disc herniation
2) Spondylosis
3) Spondylolisthesis
4) Facet arthropathy
5) Spinal cord impingement
6) Disc degeneration
7) Bone spurs
8) Meniscus tears
9) Rotator cuff tears
10) Shoulder joint arthritis
11) Knee joint osteoarthritis
12) Loss of cartilage
13) Cubital tunnel syndrome
14) Carpal tunnel syndrome
15) Lateral epicondylitis, and
16) Brachial plexus impingement
to name a few.
From L&I’s standpoint, these diagnoses are challenging. That’s because their cause is rarely a single trauma or injury. Therefore, when a provider identifies the diagnosis, L&I immediately starts questioning causation. At times, L&I asks the attending provider for an opinion about causation. But, very often, L&I calls for an independent medical exam (IME) instead.
Independent medical exam
Most IME doctors find that these kinds of diagnoses do not relate to your L&I claim. There are exceptions, but they are rare. The opinions of IME doctors usually read something like this:
“Diagnosis is pre-existing and unrelated to the industrial injury for which this claim was filed.”
The reason is that most of these conditions have other causes. They include:
a) Natural aging
b) Genetics
c) Gender
d) Weight
e) Diabetes
f) Alcohol use
g) Use of tobacco.
In short, it’s easy for IME doctors to blame the cause on reasons that do not relate to the L&I claim. Unfortunately, in my opinion, IME doctors err and attribute causes to pre-existing conditions too often.
Pre-existing conditions and IME reports
Personally, I take issue with these IME opinions. They completely ignore the laws on pre-existing conditions. Legally, there can be more than one cause for a medical condition. An industrial injury may aggravate or worsen a pre-existing condition. It doesn’t matter whether the pre-existing condition was symptomatic before the work injury. If the work injury causes worsening, then the condition is causally related under the L&I claim. Yet, IME doctors rarely include this in their analysis. They just indicate that a condition is pre-existing. Thus, according to IME doctors, it’s unrelated to the L&I claim.
Segregation order
Eventually, L&I receives the IME report. In turn, L&I will likely issue an order stating it isn’t responsible for the condition. We call this a “segregation order”. Meaning, L&I has segregated the condition from the workers comp claim.
If you receive a segregation order, it’s a good idea to consult with an L&I attorney. Disagreements over causation are one of the most common issues in L&I claims. You have to appeal this decision to the Board of Industrial Insurance Appeals for resolution. Most likely, you’ll want an attorney by your side for the appeal.